Effective infection prevention and control in healthcare settings relies heavily on staff training. While there are other factors to be considered, staff who have been thoroughly trained to prevent and control infection are in the vanguard of maintaining sterility in healthcare settings.
Nosocomial infections (those acquired through healthcare delivery) can be prevented with trained staff in place. However, their role is fortified by the application of on-site protocols, signage, and monitoring. Education is only the beginning of infection prevention and control (IPC).
History of IPC
Infection prevention and control, while it’s difficult to believe, has only been part of the healthcare scene in the USA since the 1950s. But it was in the 19th Century when Dr. Ignaz Semmelweis identified handwashing as the frontline of infection control.
In 1846, Semmelweis noted that the rate of mortality among women giving birth was lower for those whose babies had been delivered by midwives than it was for those attended by medical students.
Students would move directly to obstetrics from the autopsy lab. So, Semmelweis concluded that handwashing would reduce mortality by eliminating vestigial cadaverous remains on the students’ hands. The medical community of Dr. Semmelweis’s day bridled. But today, he is fully vindicated.
We know today that the leading cause of nosocomial infections is poor hand hygiene. Nosocomial infections, if not prevented and controlled, can be the source of large-scale viral outbreaks.
The Modern War on Infection
In 2022, the WHO released the first international report on Infection Prevention and Control, highlighting the importance of hand hygiene and other simple, low-cost IPC measures capable of reducing nosocomial infections (HIAs – hospital acquired infections) by 70%. But hand hygiene, while a core IPC practice, is just the beginning.
Establishing strict protocols around the frequency of hand washing, instances when it’s required of staff, patients, and visitors, and close monitoring to ensure that these guidelines are followed consistently, are the mission of every individual healthcare facility. This is the frontline of controlling the spread of infections that may not be treatable with antibiotics if their proliferation is enabled.
The Role of Staff and Their Training in IPC
Photo by National Cancer Institute on Unsplash
One of the most important aspects of staff training in IPC is leadership. Every staff member is part of creating an environment in which the health of staff, patients, and visitors is protected to the fullest extent possible. Leading by example is effective but so is ensuring that visitors and patients in healthcare settings are as engaged in IPC as staff are. This is leadership that reaches beyond the borders of healthcare provision, enlisting the greater society in the work of preventing and controlling infection.
Scrubs are a key area in need of attention. Washing machines must be capable of sanitizing uniforms of all types worn in healthcare settings, from Skecher’s uniforms to surgical gowns. Staff should be actively prevented from wearing hospital uniforms outside the facility. This should be the case down to the sweat-absorbent socks professionals wear. Any uniform or piece of clothing worn may have made contact with bodily fluids carrying contagious pathogens.
Acting locally and thinking globally is necessary to ensure that countries with fewer healthcare resources aren’t left behind on IPC training. Our world is globalized, meaning that interest in IPC should be internationally addressed, extending the benefit of thorough training to nations with fewer resources to allocate to the project of effective IPC. Without detailed staff training, there is no IPC. But education doesn’t stop at healthcare professionals.
Patient and Visitor Education
Photo by Daniel Frank on Unsplash
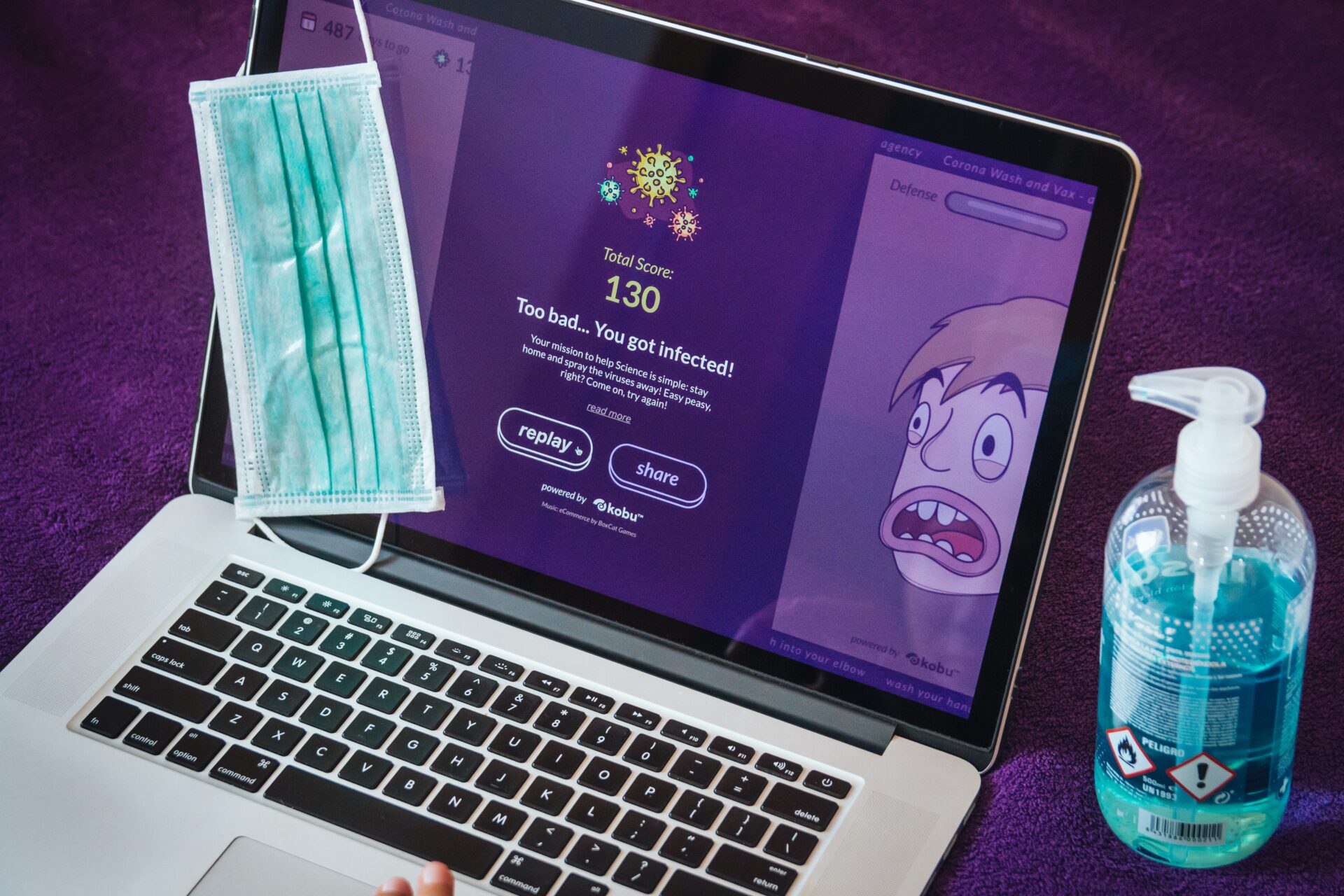
Without engaging patients and visitors in the project of IPC, healthcare professionals work in a vacuum. Just as wearing a mask is required by all when stopping the spread of a virus, so all must be engaged in the prevention and control of infection in healthcare settings.
Health literacy for patients is key to preventing infections in healthcare settings and that starts at intake. Patients should be monitored at admission to determine infection status and then, brought up to speed on behaviors required of them while in hospital. To this end, a visit from a volunteer, an orderly, or a nurse trainee well-versed in IPC, engages and empowers the patient. Contributing to the patient’s understanding leads to better outcomes offered by low infection rates.
Visitors can be similarly engaged by different means. Signage and staff assigned to inform visitors about IPC as they arrive, bring hospital visitors into the healthcare sphere as allies united in the war on infection. At the root of educating patients and visitors is an ongoing public health priority – controlling infections before they become public health emergencies. Everyone has skin in this game and everyone who sets foot in a hospital must be aware of the stakes in play.
IPC is a Communal Responsibility
The IPC training of healthcare staff in every existing role is to be shared to foster a greater understanding of the pressing need to prevent infection. When healthcare training becomes a public service announcement, IPC is served. When IPC is served, public health is defended.